Borderline personality disorder (BPD) is a mental health condition. You may have extreme mood swings, unstable relationships and trouble controlling your emotions. You have a higher risk of suicide and self-destructive behaviors. Talk therapy is the main treatment for BPD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Borderline personality disorder (BPD) is a mental health condition that affects your ability to regulate your emotions. You may experience periods of feeling intense and often uncontrollable emotions after a triggering event. As a result, it can affect the way you see yourself and cause you to act impulsively, which can disrupt relationships in your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Each person’s experience with BPD is different. You might not see yourself positively or hold yourself with confidence. You may self-sabotage by failing a test intentionally or not showing up to work. You may view others in extremes and quickly change your opinion of them. You may cling to others due to a strong fear of abandonment. Or you might drive recklessly or self-harm without thinking about the consequences of your actions.
Borderline personality disorder is one of a group of conditions called “Cluster B” personality disorders. These are chronic (long-term) conditions that cause unstable moods and emotions, impulsive behaviors and social dysfunction.
These behaviors may seem normal to you because it’s how part of your brain is wired. But the location of these wires isn’t permanent. A healthcare provider can help you find healthier ways to manage your emotions.
BPD affects an estimated 1 out of every 100 people in the United States.
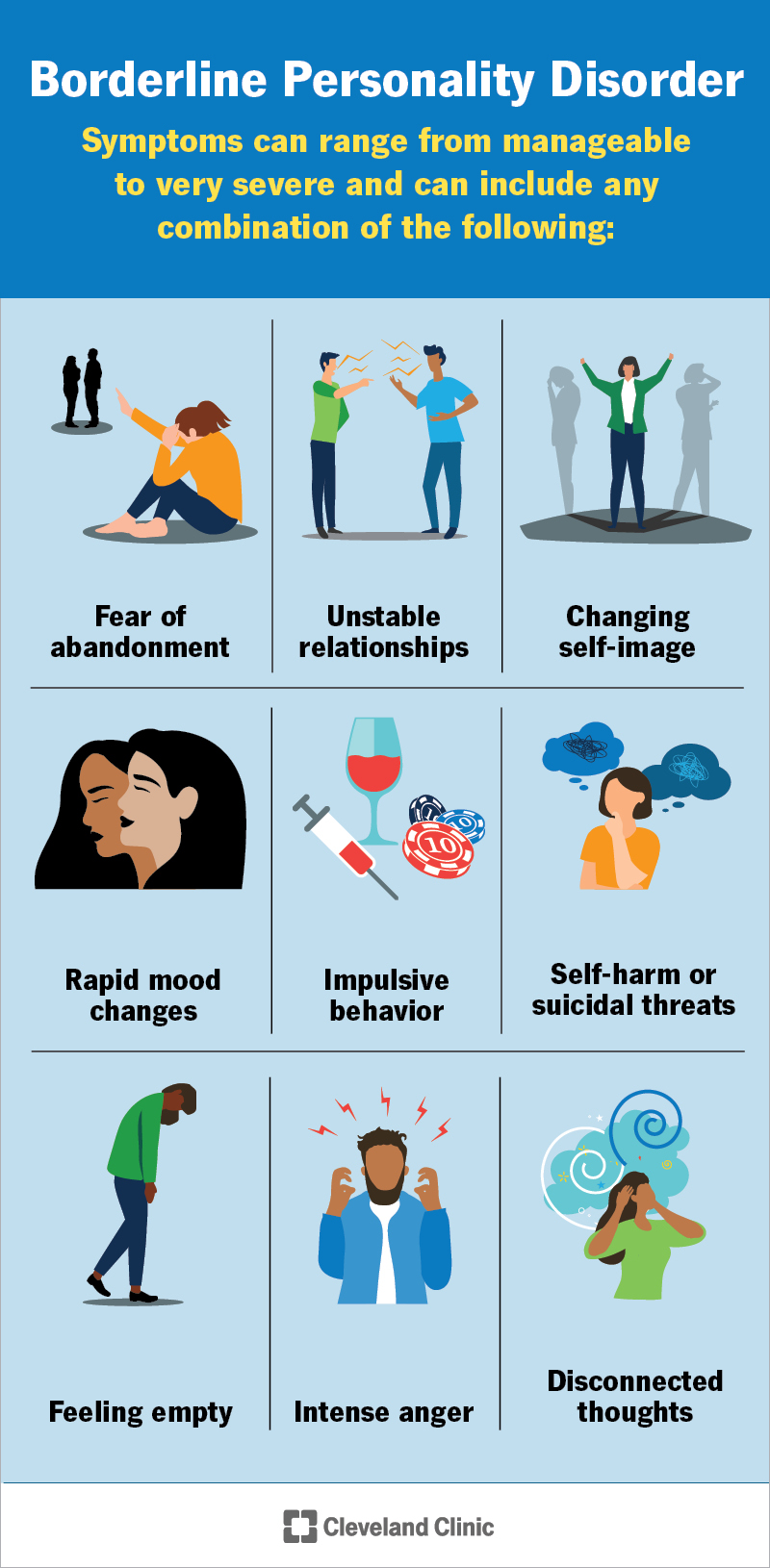
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9762-borderline-personality-disorder)
Signs and symptoms of BPD can range from manageable to very severe. They include any combination of the following:
Advertisement
Not everyone with borderline personality disorder experiences all of these symptoms. The severity, frequency and duration of symptoms are unique to each person.
Adverse childhood experiences may contribute to the development of borderline personality disorder. Common negative experiences may include, but aren’t limited to, the following:
In some cases, the parts of your brain responsible for emotion and behavior may have trouble communicating as expected. This could lead to BPD symptoms.
Although anyone can develop BPD, it’s more common if you:
Most diagnosed cases of BPD affect females. Research suggests that males may be equally affected by BPD. Unfortunately, males may be misdiagnosed with another mental health condition like post-traumatic stress disorder (PTSD) or depression.
Unfortunately, there’s no way to prevent borderline personality disorder.
Is borderline personality disorder genetic?
You may have a higher risk of developing borderline personality disorder if it runs in your biological family. BPD is five times more common if you have a first-degree relative, like a biological parent or sibling, diagnosed with the condition.
Borderline personality disorder can affect your emotional well-being. You may be more at risk of developing other mental health conditions like depression, anxiety, eating disorders or substance use disorder.
BPD can significantly impact your personal life, especially if it goes undiagnosed or untreated. You might have unstable or chaotic personal relationships and have trouble keeping a job. You may also have an increased risk of divorce, estrangement from family members and rocky friendships. Legal and financial problems are also common.
Your risk of death by suicide increases significantly with borderline personality disorder. You may be more likely to self-harm or to take risks without thinking about the possible outcomes, even if they could be life-threatening.
A mental health professional, like a psychiatrist or a psychologist, can diagnose this condition. They’ll compare your symptoms with the diagnostic criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
There isn’t a single BPD test to diagnose it. Instead, your provider will perform a thorough interview and discuss your symptoms. They’ll ask questions that’ll shed light on:
Advertisement
Your provider will evaluate the severity of your symptoms during the initial diagnosis. This can help them create a treatment plan that best fits your needs.
Personality disorders can be difficult to diagnose, as you may not see your behavior or thought patterns as disruptive. Mental health professionals often work with your family and friends to collect more insight into your behaviors and history.
As your personality continues to evolve throughout childhood and adolescence, providers don’t typically diagnose BPD until after age 18. Occasionally, a person younger than 18 may receive a diagnosis if symptoms are significant and last at least a year.
After your provider makes a diagnosis, they’ll help you learn more about BPD and what this means for you. They’ll clear up any misconceptions about the condition because it isn’t always presented accurately in shows or movies. Then, they’ll work with you to discuss the next steps in your treatment plan.
Your provider will recommend psychotherapy or talk therapy for borderline personality disorder. The goal of treatment is to help you uncover the motivations and fears associated with your thoughts and behavior and to help you learn to relate to others more positively.
Advertisement
There are different types of therapy that may help treat BPD, including:
Your healthcare provider may recommend a short-term hospital stay if you’re very distressed or at risk of harming yourself or others. This stay is designed to keep you safe. Your care team will help you create a treatment plan so you have the resources you need when you leave the hospital.
Advertisement
Because the benefits of prescription medication for borderline personality disorder are unclear, healthcare providers typically don’t prescribe medications as the main treatment for BPD.
If your provider recommends a medication, it’ll be time-limited to address a specific symptom you experience. It also won’t be prescribed alone. You’ll need to participate in psychotherapy while taking the medication to see its effectiveness. Your provider may review or change the medications you take every six months to make sure it’s working.
In some cases, a provider may recommend medications to treat other mental health conditions. Medications are available for anxiety, depression and bipolar disorder, among others.
Due to the intense emotions you feel, your risk of harming yourself or attempting suicide is much higher than others.
If you’re thinking about suicide, know that there are people available 24/7 who can help you through whatever you’re dealing with at that moment. You can call or text 988. This is the Suicide & Crisis Lifeline (U.S.). You don’t have to be in a crisis to talk to someone.
If you’re in immediate danger, call 911 or your local emergency services number.
Borderline personality disorder is a lifelong mental health condition. Even though symptoms may gradually decrease with age, usually around 40, you shouldn’t wait for your symptoms to fade. This is because the rippling effects of your emotions and behavior may significantly impact you for more than just the length of time when you have them.
With the right treatment, you can learn skills to manage your emotions and behavior in a healthy way that can benefit you for a lifetime.
If symptoms continue without an accurate diagnosis and treatment, it may affect your life expectancy due to the risk of suicide and self-harming behaviors.
BPD historically has been challenging to treat. But with newer, person-centered treatment plans, many people with BPD experience fewer and less severe symptoms, improved functioning and better quality of life.
Your emotions might feel like they’re on a seesaw, teetering back and forth unpredictably with borderline personality disorder (BPD). This mental health condition can take a significant toll on your relationships and personal life. But help is available.
Effective treatment takes time, patience and commitment. It doesn’t happen overnight. Your care team will be with you every step of the way. They can offer support and help you stay on track so you can meet your goals. Let your providers know if you have any questions about your treatment plan or what you can expect with a BPD diagnosis.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Your mental well-being is just as important as your physical well-being. Cleveland Clinic’s mental health experts can help you live life to the fullest.
